Sacral Colpopexy Procedure with synthetic mesh
Overview for prolapse surgery using MESH
The first line of SURGICAL treatment for prolapse repair is to use the patient’s OWN native tissue. However, if the patient’s own tissue is TOO WEAK and/or she develops recurrent prolapse or if the patients prolapse is SEVERE (e.g. Stage IV prolapse), then the next step would be the Sacral Colpopexy procedure.
The second line and GOLD STANDARD treatment for recurrent prolapse is the sacral colpopexy procedure with SYNTHETIC MESH. With recurrent prolapse and weak fascial tissue, the risk of recurrent prolapse is very high. Using the patient’s own tissue again for a second repair would be unsuccessful, so the next step will be to use synthetic mesh as a replacement for the patient’s own weak fascial tissue. My preferred synthetic mesh is a macroporous, monofilament, polypropylene mesh. I prefer the Restorelle mesh or the Upsylon Y shaped mesh. The image below is characteristics of this monofilament, macroporous, synthetic mesh.

TWO main indications for a Sacral Colpopexy procedure?
a. Patient’s own tissue is TOO WEAK and she has a FAILED prior prolapse repair. Now, she has recurrent prolapse. The most common scenario is a patient who has had a prior hysterectomy with a bulge that is protruding outside the vaginal opening.
b. Severe prolapse (e.g. Stage IV prolapse) where the prolapse bulge is protruding 6-8 cm OUTSIDE the opening of the vaginal introitus.

STEPS of the sacral colpopexy procedure
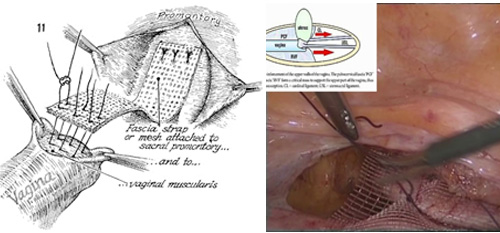
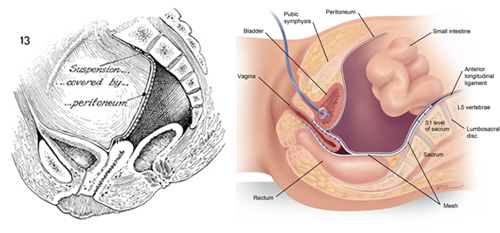
The goal of the procedure is to use additional tissue, specifically synthetic mesh to reinforce the support of the surgical procedure. Typically, I use a Y-shaped monofilament polypropylene synthetic mesh that provides support for all THREE compartments of the vaginal canal, specifically the anterior compartment (e.g. bladder compartment), apical compartment (e.g. top of the vaginal canal), and the posterior compartment (e.g. the rectocele compartment). This Y-shaped mesh is anchored to the anterior ligaments of the sacral promontory area (e.g. tailbone). The analog is that any wall painting needs to be anchored to the WALL STUD for better long-term support.
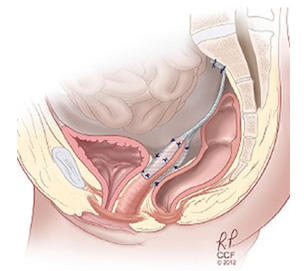
First, you need to dissect the bladder off the anterior vaginal compartment, approximately 6-7 cm in length along the anterior compartment. The same procedure is performed along the posterior vaginal compartment (e.g. rectocele compartment)
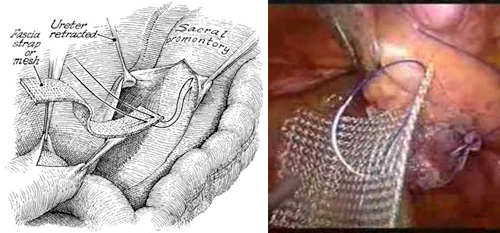
Then a dissection is performed along the sacral promontory area to identify the anterior ligament of the sacrum.
After the sacral colpopexy procedure, the mesh is re-peritonealized and completed covered with no mesh showing.
Risks of the sacral colpopexy procedure?
There are many limitations of this sacral colpopexy procedure. When a synthetic mesh / foreign body is uses. There is risks for mesh are:
a. Mesh erosion
b. Mesh infection
c. Mesh pain
d. And other complications, like bleeding, and mesh pulling sensation at the mesh site.
OVERALL, the sacral colpopexy procedure is a procedure of last resort and GOLD STANDARD for recurrent prolapse. We only consider the sacral colpopexy procedure AFTER the patient has FAILED pessary management and FAILED prior prolapse repair using her own tissue.
Post op recovery
The two main limitations during the sacral colpopexy procedure are:
a. No heavy lifting (x < 15 lbs.) for 3 months post-surgery
b. Showers only. No baths, no pools, no intimacy, and no soaking in any water for 2 months post-surgery. Overall, each patient heals at their own rate, so each patient needs to listen to her body, with activity as tolerated.
c. Full recovery and return to normal activities in approximately 6 weeks.